03 Jan Retinal Detachment
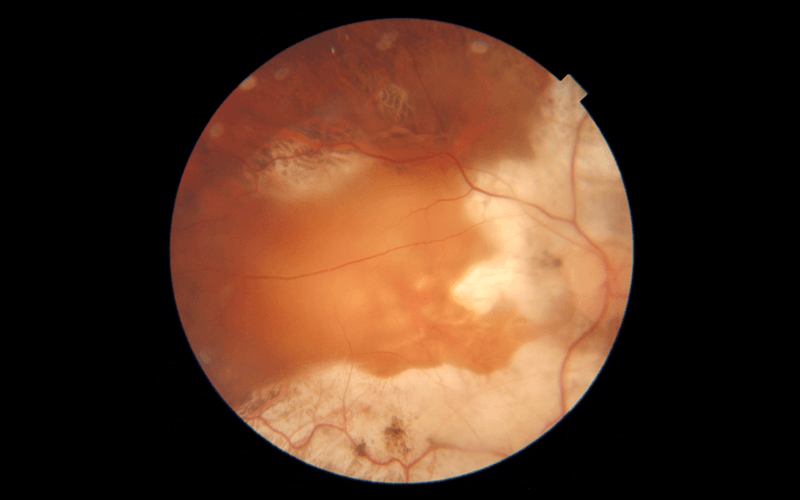
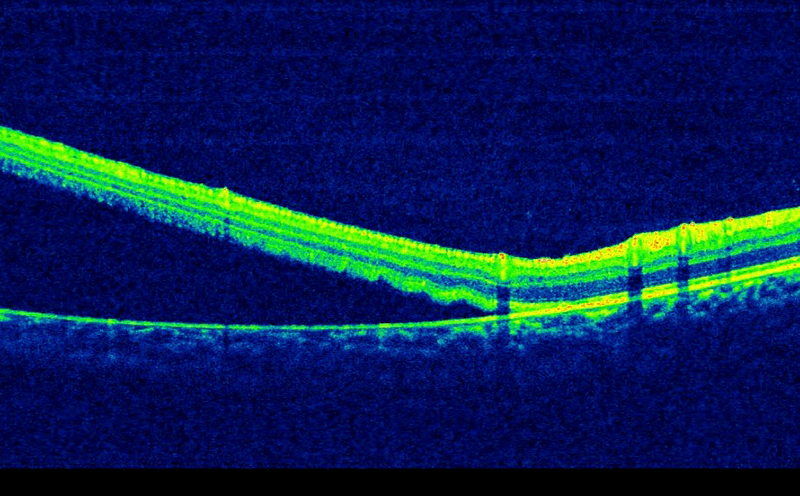
Vitreous gel, the clear material that fills the eyeball, is attached to the retina in the back of the eye. As we get older, the vitreous may shrink, pulling away from the retina. Rarely, the vitreous pulls a piece of the retina with it, causing a retinal tear. Once a retinal tear occurs, vitreous fluid may seep through and lift the retina off the back wall of the eye (as wallpaper can peel off a wall), causing the retina to detach.
The retina does not work when it is detached and vision becomes blurry. A retinal detachment is a very serious problem that causes blindness unless it is treated with surgery.
Risk Factors:
- Myopia (high minus numbers)
- Previous eye surgery
- Severe eye injury
- Retinal detachment in the other eye
- Family history of retinal detachment
- Weak areas in the retina that can be seen by an ophthalmologist during an eye exam
Those having risk factors should have complete dilated eye exams on a regular basis. It is better to wear protective eyewear when playing sports and in case of a serious eye injury, retina specialist should be consulted right away.
Warning symptoms include:
- A sudden increase in size and number of floaters
- A sudden appearance of flashes
- Having a shadow (grey curtain) appear in the periphery (side) of the field of vision;
- A sudden decrease in vision
A dilated examination can diagnose retinal tear or retinal detachment. An ultrasound of the eye may also be performed to get additional detail of the retina.
Retinal tear treatment
Retinal tears are treated with laser beams. It creates a scar that helps seal the retina to the back of the eye. This usually prevents the retina from detaching.
Detached retina surgery
A detached retina is repaired with a surgical procedure. Based on various factors, the retina specialist discusses the type of procedure recommended taking into account the risks and benefits of each option.
Scleral buckle
This involves placing a flexible band (scleral buckle) around the eye to counteract the force pulling the retina out of place. The fluid under the detached retina may be drained or left for the body to absorb. This allows the retina to settle back into its normal position.
Pneumatic retinopexy
A few selected cases may be suitable for this type of procedure. In this, a gas bubble is injected into the vitreous space inside the eye in combination with laser treatment or cryotherapy (freezing treatment). The gas bubble pushes the retinal tear into place against the back wall of the eye. It is essential to constantly maintain a certain head position for several days. The gas bubble gradually disappears.
Vitrectomy
In this, the vitreous gel, which is pulling on the retina, is removed from the eye and usually replaced with a gas or oil bubble. While a gas bubble gets absorbed on its own, an oil bubble will need to be removed from the eye at a later date with another surgical procedure. Sometimes vitrectomy is combined with a scleral buckle.
Most retinal detachment surgeries (nearly 90 percent) are successful, although a second operation is sometimes needed. Some retinal detachments cannot be fixed. The development of scar tissue is the usual reason that a retina is not able to be fixed. If the retina cannot be reattached, the eye will continue to lose sight and ultimately become blind.
Even after a successful surgery for retinal detachment, vision may take many months to improve and, in some cases, may never return fully. Unfortunately, some patients do not recover any vision. The more severe the detachment and more delayed the treatment, the less vision may return. For this reason, it is very important to see your ophthalmologist regularly or at the first sign of any trouble with your vision.


Sorry, the comment form is closed at this time.